Hi
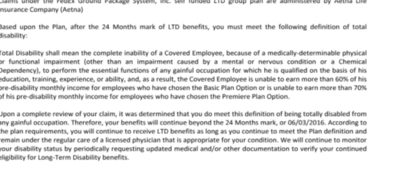
My wife has been on LTD since 2015. Initially the LTD was administered by Aetna and now The Hartford. My wife has a severe mental illness(schizophrenia) which her company stated was NOT subject to the 24 month mental illness LTD limitation. This was confirmed in an email correspondence with the company's leave management specialist..She also has been on SSDI since 2015. Aetna did a full review in 2017 and determined that she is totally disabled and her LTD will continue.
The Hartford has administered the plan since 2017 and I received a call last week stating that her LTD should have ended after the 24 month mental health limitation and they will be seeking overpayment since 2015. Of course i was shocked and my wife is a nervous wreck . I probably will have to seek legal advice but I would greatly appreciate any suggestions on what to do.
thanks in advance
My wife has been on LTD since 2015. Initially the LTD was administered by Aetna and now The Hartford. My wife has a severe mental illness(schizophrenia) which her company stated was NOT subject to the 24 month mental illness LTD limitation. This was confirmed in an email correspondence with the company's leave management specialist..She also has been on SSDI since 2015. Aetna did a full review in 2017 and determined that she is totally disabled and her LTD will continue.
The Hartford has administered the plan since 2017 and I received a call last week stating that her LTD should have ended after the 24 month mental health limitation and they will be seeking overpayment since 2015. Of course i was shocked and my wife is a nervous wreck . I probably will have to seek legal advice but I would greatly appreciate any suggestions on what to do.
thanks in advance